Touro College of Dental Medicine
Contact
Hours
- Monday: 9:00am – 9:00pm
- Tuesday: 9:00am – 6:00pm
- Wednesday: 9:00am – 9:00pm
- Thursday: 9:00am – 9:00pm
- Friday: 9:00am – 5:00pm
Touro College of Dental Medicine, located in New York, New York, is a distinguished institution dedicated to providing exceptional dental education, advancing research in the field of dentistry, and delivering compassionate patient care. As a leading dental school, we are committed to preparing competent and compassionate dental professionals who will serve their communities with integrity and excellence. Our faculty comprises esteemed educators and researchers who are passionate about fostering the next generation of dental leaders and advancing oral health for all.
Educational Programs
Dental Degree Programs
- Doctor of Dental Surgery (DDS): Comprehensive program designed to provide students with a solid foundation in dental science, clinical skills, and professional ethics.
- Advanced Dental Education: Postgraduate programs offering specialized training in areas such as orthodontics, periodontics, endodontics, and oral surgery.
Continuing Education
- Professional Development: Continuing education courses and seminars for practicing dentists to enhance their clinical skills, stay updated on the latest advancements in dental research, and meet licensure requirements.
- Specialized Training: Advanced training programs for dental specialists seeking to further develop their expertise in specific areas of dentistry.
Clinical Services
Patient Care
- Comprehensive Dental Care: Range of preventive, restorative, and cosmetic dental services provided by faculty-supervised students and experienced dental professionals.
- Specialty Care: Specialized treatment options for complex dental conditions, including orthodontics, periodontics, endodontics, and oral surgery.
Community Outreach
- Public Health Initiatives: Collaborative efforts with community organizations to promote oral health education, provide dental screenings, and deliver preventive services to underserved populations.
- Community Service: Participation in outreach programs and volunteer initiatives to address the oral health needs of underserved communities and improve access to dental care.
Research and Innovation
Scientific Inquiry
- Translational Research: Conducting cutting-edge research to translate scientific discoveries into clinical applications for improved patient care and outcomes.
- Interdisciplinary Collaboration: Collaborating with other academic institutions and research centers to advance knowledge in various areas of dental science and medicine.
Touro College of Dental Medicine is dedicated to excellence in dental education, research, and patient care, serving the needs of individuals and communities in New York and beyond. Through our commitment to academic excellence, clinical innovation, and community engagement, we strive to make a positive impact on oral health and well-being for generations to come.
Overdentures
Overdentures, also known as implant-supported dentures or removable implant-supported dentures, are a type of dental prosthesis that is supported by dental implants. Unlike traditional dentures, which rest on the gums and rely on suction or adhesive for retention, overdentures are anchored securely to dental implants, providing increased stability, support, and functionality. Here's an overview of overdentures:
- Indications:
- Overdentures are often recommended for patients who have lost all or most of their natural teeth and have insufficient bone density or quality to support fixed dental implants or bridges.
- They are particularly beneficial for patients who struggle with loose, uncomfortable, or poorly fitting traditional dentures, as overdentures offer improved stability, retention, and comfort.
- Implant Placement:
- The first step in the overdenture process involves the placement of dental implants in the jawbone. The number and location of implants vary depending on factors such as bone density, jaw anatomy, and the specific requirements of the case.
- Typically, a minimum of two to four implants are placed in the jawbone to support an overdenture. In some cases, additional implants may be placed for increased stability and support.
- Healing and Osseointegration:
- After implant placement, a healing period of several months is usually required to allow for osseointegration, the process by which the implants fuse with the surrounding bone tissue.
- During this time, temporary restorations may be worn to maintain aesthetics and function while the implants heal and integrate with the jawbone.
- Prosthesis Fabrication:
- Once osseointegration is complete, the dental implants are ready to support the overdenture.
- The overdenture is custom-made to fit securely over the dental implants and restore function and aesthetics. It may be fabricated from acrylic, composite resin, or a combination of materials.
- Special attachments or connectors are used to secure the overdenture to the implants, providing stability and retention while still allowing for easy removal and cleaning.
- Placement and Adjustment:
- The overdenture is placed and adjusted by the dentist to ensure proper fit, comfort, and function.
- The dentist will check the bite, occlusion, and aesthetics of the overdenture to ensure that it meets the patient's expectations.
- Any necessary adjustments or modifications are made to optimize the fit and comfort of the overdenture.
- Postoperative Care and Maintenance:
- After the overdenture is placed, the patient will receive instructions on postoperative care and maintenance.
- Good oral hygiene practices, including daily brushing, flossing, and regular dental check-ups, are essential for maintaining the health of the implants and surrounding tissues.
- The overdenture should be removed and cleaned regularly to prevent plaque buildup, bacterial growth, and irritation of the gums.
Overdentures offer several advantages over traditional dentures, including improved stability, retention, and chewing efficiency. They can enhance the quality of life for patients with missing teeth by restoring oral function, aesthetics, and confidence. If you are considering overdentures as a treatment option, it's important to consult with a qualified dentist or prosthodontist to determine the best treatment plan for your individual needs.
Lingual Tonsillitis
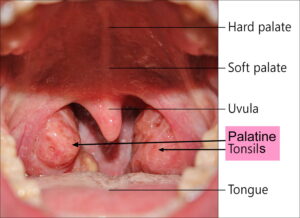
Lingual tonsillitis is an inflammatory condition that affects the lingual tonsils, which are clusters of lymphoid tissue located at the base of the tongue. Similar to the palatine tonsils (commonly referred to as the tonsils), the lingual tonsils play a role in the immune system's defense against infections.
Here are some key points about lingual tonsillitis:
- Causes: Lingual tonsillitis is typically caused by viral or bacterial infections. Common viral pathogens responsible for lingual tonsillitis include the Epstein-Barr virus (EBV), adenovirus, or influenza virus. Bacterial infections, particularly streptococcal bacteria (such as Streptococcus pyogenes), can also cause lingual tonsillitis. Other potential causes include fungal infections, allergies, or irritants (such as smoking or environmental pollutants).
- Symptoms: The symptoms of lingual tonsillitis are similar to those of tonsillitis affecting the palatine tonsils. These may include sore throat, difficulty swallowing (dysphagia), pain or discomfort at the back of the tongue, swollen or enlarged lingual tonsils, redness or inflammation of the throat, fever, headache, or swollen lymph nodes in the neck.
- Diagnosis: Diagnosis of lingual tonsillitis involves a thorough medical history, physical examination, and evaluation of symptoms. The healthcare provider may examine the back of the throat and base of the tongue using a lighted instrument called a tongue depressor or perform a throat culture or swab to identify the causative organism. Imaging studies such as CT scan or MRI may be ordered in cases of severe or recurrent lingual tonsillitis to assess for complications or underlying structural abnormalities.
- Treatment: Treatment of lingual tonsillitis aims to alleviate symptoms, eliminate the underlying infection, and prevent complications. This may involve conservative measures such as rest, hydration, warm saltwater gargles, throat lozenges, or over-the-counter pain relievers (such as ibuprofen or acetaminophen) to relieve discomfort. In cases of bacterial infection, antibiotic therapy may be prescribed. For fungal infections or severe cases of lingual tonsillitis, antifungal medications or corticosteroids may be recommended.
- Complications: If left untreated, lingual tonsillitis can lead to complications such as peritonsillar abscess (collection of pus near the tonsils), retropharyngeal abscess (infection in the deep tissues of the neck), or airway obstruction due to swelling of the lingual tonsils. Prompt diagnosis and appropriate treatment are essential to prevent complications and promote recovery.
In summary, lingual tonsillitis is an inflammatory condition affecting the lingual tonsils, characterized by symptoms such as sore throat, difficulty swallowing, and swollen lingual tonsils. Treatment typically involves conservative measures and, in some cases, antibiotic therapy to eliminate the underlying infection and alleviate symptoms. Prompt medical attention is important to prevent complications and promote recovery.