Barnet Health Doctors
Contact
Hours
- Monday: 9:00am – 9:00pm
- Tuesday: 9:00am – 6:00pm
- Wednesday: 9:00am – 9:00pm
- Thursday: 9:00am – 9:00pm
- Friday: 9:00am – 5:00pm
Barnet Health Doctors, located in the charming town of Middletown, New York, is a premier dental institution dedicated to providing comprehensive and compassionate dental care to patients of all ages. With a focus on oral health and wellness, the practice is committed to delivering high-quality dental services in a warm and welcoming environment. Led by a team of skilled dental professionals, Barnet Health Doctors offers a wide range of dental treatments to help patients achieve and maintain healthy smiles.
Dental Services
Preventive Dentistry
- Comprehensive Examinations: Thorough dental examinations to assess oral health and detect any signs of dental problems.
- Professional Cleanings: Routine cleanings to remove plaque and tartar buildup, helping to prevent gum disease and cavities.
- Dental Sealants: Protective coatings applied to the chewing surfaces of molars to prevent decay and cavities in children and adults.
Restorative Dentistry
- Fillings: Treatment of cavities with tooth-colored composite fillings for a natural-looking restoration.
- Crowns and Bridges: Custom-made dental crowns and bridges to restore and strengthen damaged or missing teeth.
- Dentures: Complete or partial dentures to replace missing teeth and restore oral function and aesthetics.
Specialized Dental Care
Orthodontics
- Braces: Traditional metal braces and clear aligner therapy to straighten teeth and correct bite issues.
- Retainers: Custom-made retainers to maintain the alignment of teeth following orthodontic treatment.
Endodontics
- Root Canal Therapy: Treatment to save and repair infected or damaged teeth by removing infected pulp and sealing the root canal.
- Apicoectomy: Surgical procedure to remove the tip of the tooth root and seal the root canal to treat persistent infections.
Patient Care
Personalized Treatment Plans
- Individualized Consultations: Thorough discussions and treatment planning sessions to address each patient’s unique dental needs and goals.
- Collaborative Approach: Working closely with patients to develop treatment plans that fit their lifestyle and budget.
Comfort and Convenience
- Relaxing Environment: A welcoming atmosphere designed to help patients feel at ease during their dental visits.
- Pain Management: Utilization of advanced anesthesia techniques to ensure patient comfort during procedures.
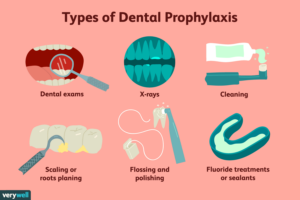
Prophylaxis
Dental prophylaxis, commonly referred to as a dental cleaning, is a preventive dental procedure performed by a dental hygienist or dentist to remove plaque, tartar (calculus), and stains from the teeth and gums. It plays a crucial role in maintaining optimal oral health and preventing dental problems such as tooth decay, gum disease, and bad breath. Here's an overview of dental prophylaxis and its importance:
- Plaque and Tartar Removal:
- Dental prophylaxis involves the thorough removal of plaque and tartar buildup from the tooth surfaces, especially along the gumline and between the teeth. Plaque is a sticky film of bacteria that forms on the teeth throughout the day and can harden into tartar if not removed through regular brushing and flossing. Tartar is a hardened deposit that cannot be removed with regular brushing and requires professional intervention to prevent dental problems.
- Prevention of Tooth Decay and Gum Disease:
- By removing plaque and tartar, dental prophylaxis helps prevent the development of tooth decay (cavities) and gum disease (periodontal disease). Plaque bacteria produce acids that can erode tooth enamel and lead to cavities, while tartar buildup along the gumline can irritate the gums and contribute to gum inflammation and infection. Regular dental cleanings help keep the teeth and gums healthy and reduce the risk of dental problems.
- Detection of Oral Health Issues:
- During a dental cleaning, the dental hygienist or dentist will also perform a thorough examination of the teeth, gums, and oral tissues to detect any signs of dental problems or oral health issues. This may include checking for signs of tooth decay, gum inflammation, oral cancer, or other abnormalities. Early detection and intervention are key to preventing the progression of oral health issues and maintaining overall oral health.
- Fresh Breath:
- Dental prophylaxis can also help improve and maintain fresh breath by removing plaque, tartar, and bacteria that contribute to bad breath (halitosis). Cleaning the teeth and gums thoroughly can eliminate odor-causing bacteria and leave the mouth feeling clean and refreshed.
- Promotion of Overall Health:
- Research has shown that there is a strong link between oral health and overall health, with poor oral hygiene being associated with an increased risk of systemic health problems such as heart disease, diabetes, and respiratory infections. By maintaining good oral hygiene habits and scheduling regular dental cleanings, individuals can help protect their overall health and well-being.
Overall, dental prophylaxis is an essential component of preventive dental care that helps keep the teeth and gums healthy, prevents dental problems, and promotes overall oral and systemic health. It is recommended that individuals undergo dental cleanings at least every six months, or as recommended by their dentist, to maintain optimal oral health and prevent the need for more extensive dental treatment in the future.
Papilloma
A papilloma is a benign epithelial tumor or growth that typically arises from the skin or mucous membranes. In the context of oral health, papillomas can occur in various locations within the oral cavity, including the lips, tongue, palate, cheeks, or gums. Oral papillomas are often caused by infection with human papillomavirus (HPV), particularly certain high-risk strains such as HPV types 6 and 11.
Here are some key points about oral papillomas:
- Types: Oral papillomas can be classified into several subtypes based on their clinical and histological features:
- Squamous papilloma: This is the most common type of oral papilloma and typically presents as a small, painless, pedunculated (stalk-like) or sessile (flat) growth on the oral mucosa. Squamous papillomas are usually pink or white in color and have a cauliflower-like appearance due to the presence of finger-like projections or papillary structures.
- Verruca vulgaris (common wart): Although more commonly found on the skin, verruca vulgaris can also occur in the oral cavity and present as papillomatous growths with a rough or hyperkeratotic surface.
- Condyloma acuminatum: This subtype of oral papilloma is associated with HPV infection and typically occurs in the anogenital region. However, it can rarely affect the oral mucosa, particularly in individuals with immunodeficiency or compromised immune function.
- Etiology: Oral papillomas are often caused by infection with HPV, a common sexually transmitted virus that can infect the skin and mucous membranes. HPV types 6 and 11 are most commonly associated with oral papillomas, particularly squamous papillomas. Transmission of HPV can occur through direct contact with infected skin or mucous membranes, including oral-genital contact or autoinoculation from other sites of infection.
- Symptoms: Oral papillomas are typically painless and may go unnoticed until they become enlarged or bothersome. Depending on their size and location, papillomas may cause discomfort, irritation, or a sensation of a foreign body in the mouth. In some cases, papillomas may bleed or become ulcerated if traumatized.
- Diagnosis: Diagnosis of oral papillomas is typically based on clinical examination and evaluation of the characteristic appearance and location of the lesion. In some cases, a biopsy may be performed to confirm the diagnosis and rule out other potential causes of oral growths.
- Treatment: Treatment of oral papillomas usually involves surgical excision or removal of the lesion, particularly if it causes symptoms, interferes with oral function, or is cosmetically undesirable. The procedure is typically performed by a dentist or oral surgeon under local anesthesia to numb the area before removal. Recurrence of oral papillomas is possible, particularly if the underlying HPV infection is not adequately treated or if predisposing factors such as immunodeficiency are present.
In summary, oral papillomas are benign epithelial tumors or growths that typically arise from the oral mucosa and are often caused by HPV infection. While usually painless and benign, papillomas can cause discomfort or interfere with oral function if they become symptomatic or enlarging. Treatment options vary depending on the size, location, and symptoms of the papilloma but may include surgical excision or removal. Early diagnosis and appropriate management are important for preventing complications and achieving favorable outcomes.