Barnet University Hospital
Contact
Hours
- Monday: 9:00am – 9:00pm
- Tuesday: 9:00am – 6:00pm
- Wednesday: 9:00am – 9:00pm
- Thursday: 9:00am – 9:00pm
- Friday: 9:00am – 5:00pm
Barnet University Hospital, a leading healthcare institution located in New York, offers a comprehensive range of medical and dental services. This fictional hospital is renowned for its state-of-the-art facilities and commitment to providing high-quality care to all patients.
Medical Services
General Medicine and Surgery
- Emergency Services: Open 24/7, equipped with advanced life-saving technology.
- Inpatient and Outpatient Care: Comprehensive services including internal medicine, cardiology, neurology, orthopedics, and more.
- Surgical Specialties: General surgery, trauma surgery, minimally invasive procedures, and specialized surgical interventions.
Specialized Departments
- Oncology: Cutting-edge cancer treatment and research center.
- Pediatrics: Comprehensive care for infants, children, and adolescents.
- Women’s Health: Maternity services, gynecology, and reproductive health.
Dental Services
General Dentistry
- Routine Checkups and Cleanings: Preventive care to maintain oral health.
- Fillings and Restorations: Treatment of cavities and damaged teeth.
Specialized Dental Care
- Oral and Maxillofacial Surgery: Surgical extraction of teeth, removal of diseased tissue, and corrective jaw surgery.
- Orthodontics: Braces and other orthodontic treatments for children and adults to correct dental alignment and bite issues.
- Pediatric Dentistry: Specialized dental care for children, including preventive treatments like sealants and fluoride applications.
- Periodontics: Treatment of gum disease and other conditions affecting the tissues surrounding the teeth.
- Prosthodontics: Replacement of missing teeth with crowns, bridges, dentures, and dental implants.
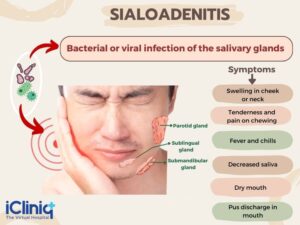
Sialadenitis
Sialadenitis is an inflammatory condition affecting one or more of the salivary glands, which are responsible for producing saliva. This inflammation can be acute or chronic and may result from infection, obstruction, autoimmune disorders, or other underlying causes.
Here are some key points about sialadenitis:
- Causes: Sialadenitis often occurs due to bacterial infection, most commonly by the bacteria Staphylococcus aureus or Streptococcus species. The infection may result from obstruction of the salivary gland ducts, which can occur due to factors such as salivary gland stones (sialolithiasis), dehydration, poor oral hygiene, or certain medical conditions (such as Sjögren's syndrome). Other causes of sialadenitis include viral infections (such as mumps), autoimmune disorders (such as Sjögren's syndrome or sarcoidosis), radiation therapy to the head and neck, or systemic conditions affecting the salivary glands.
- Symptoms: The symptoms of sialadenitis may include pain and swelling in the affected salivary gland, often worsened during meals when saliva production increases. Other common symptoms may include redness or warmth over the affected gland, fever, chills, difficulty opening the mouth, dry mouth, or foul-tasting saliva. In severe cases, abscess formation or pus drainage from the duct opening may occur.
- Diagnosis: Diagnosis of sialadenitis involves a thorough medical history, physical examination, and evaluation of symptoms. Diagnostic tests, such as ultrasound, CT scan, or MRI, may be used to visualize the salivary glands and assess for signs of inflammation, obstruction, or abscess formation. In cases of suspected bacterial infection, a culture of the saliva or pus may be obtained to identify the causative organism and guide antibiotic therapy.
- Treatment: Treatment of sialadenitis depends on the underlying cause and severity of symptoms. Acute bacterial sialadenitis is typically treated with antibiotics to eliminate the infection, along with measures to promote saliva flow (such as hydration, warm compresses, and sour candies or lemon juice). In cases of obstruction, manual expression of saliva or surgical removal of salivary gland stones may be necessary. Chronic sialadenitis may require long-term management with antibiotics, anti-inflammatory medications, or other interventions to control symptoms and prevent recurrence.
- Complications: If left untreated, sialadenitis can lead to complications such as abscess formation, cellulitis (spread of infection to surrounding tissues), or recurrent infections. In severe cases, chronic inflammation of the salivary glands may cause irreversible damage, leading to decreased saliva production and increased risk of dental decay, oral infections, or difficulty swallowing.
In summary, sialadenitis is an inflammatory condition affecting the salivary glands, typically caused by infection, obstruction, or autoimmune disorders. Prompt diagnosis and appropriate treatment are essential to alleviate symptoms, prevent complications, and preserve the function of the salivary glands.
Oral Thrush
Oral thrush, also known as oral candidiasis, is a fungal infection caused by Candida yeast species, typically Candida albicans. It commonly affects the mouth and throat, particularly the mucous membranes and moist areas such as the tongue, inner cheeks, gums, and throat. Oral thrush can cause discomfort, pain, and difficulty swallowing, and it is more prevalent in individuals with weakened immune systems, certain medical conditions, or those taking medications that disrupt the balance of microorganisms in the mouth.
Here are some key points about oral thrush:
- Causes:
- Candida overgrowth: Oral thrush occurs when there is an overgrowth of Candida yeast in the mouth, often due to factors that disrupt the natural balance of microorganisms in the oral cavity.
- Weakened immune system: Conditions that weaken the immune system, such as HIV/AIDS, diabetes, cancer, or autoimmune disorders, increase the risk of oral thrush.
- Medications: Certain medications, such as antibiotics, corticosteroids, immunosuppressants, or chemotherapy drugs, can alter the oral microbiota and predispose individuals to oral thrush.
- Hormonal changes: Hormonal fluctuations, such as those occurring during pregnancy, menopause, or hormonal therapy, can increase susceptibility to oral thrush.
- Poor oral hygiene: Inadequate oral hygiene practices, such as infrequent brushing, flossing, or denture cleaning, can contribute to the development of oral thrush.
- Smoking: Tobacco use, particularly smoking, can weaken the immune system and promote Candida overgrowth in the mouth.
- Symptoms:
- White, creamy, or yellowish patches on the tongue, inner cheeks, gums, or throat.
- Soreness, burning, or discomfort in the mouth, especially when eating or drinking.
- Difficulty swallowing or persistent throat pain.
- Loss of taste or altered taste sensation (dysgeusia).
- Cracking or redness at the corners of the mouth (angular cheilitis) in severe cases.
- Bleeding or mucosal irritation when the patches are scraped or rubbed.
- Diagnosis:
- Diagnosis of oral thrush is typically based on clinical examination and evaluation of symptoms by a healthcare professional.
- Your healthcare provider may perform a physical examination of the mouth and throat and may collect samples (swabs) from the affected areas for microscopic examination or culture to confirm the presence of Candida yeast.
- Treatment:
- Treatment of oral thrush aims to eliminate the fungal infection, alleviate symptoms, and prevent recurrence. Treatment options may include:
- Antifungal medications: Topical antifungal agents such as nystatin oral suspension or clotrimazole lozenges are commonly used to treat mild to moderate cases of oral thrush. Severe or persistent infections may require systemic antifungal medications such as fluconazole.
- Oral hygiene measures: Practicing good oral hygiene, including regular brushing, flossing, and tongue cleaning, can help reduce oral thrush symptoms and prevent recurrence.
- Denture care: Proper cleaning and maintenance of dentures or oral appliances are essential to prevent Candida overgrowth and denture-related oral thrush.
- Treatment of underlying conditions: Managing underlying medical conditions or risk factors such as diabetes, immunosuppression, or hormonal imbalances is important to prevent recurrent episodes of oral thrush.
- Prevention:
- To prevent oral thrush, it's important to:
- Maintain good oral hygiene practices, including regular brushing, flossing, and tongue cleaning.
- Limit sugar and yeast-containing foods in the diet, as these can promote Candida overgrowth.
- Use antibiotics judiciously and only as prescribed by a healthcare professional to minimize disruption of the oral microbiota.
- Avoid smoking or tobacco use, as these can weaken the immune system and increase susceptibility to oral thrush.
- Practice proper denture care, including regular cleaning, soaking, and removal at night to allow the oral tissues to breathe.
In summary, oral thrush is a fungal infection caused by Candida yeast species that commonly affects the mouth and throat. It can cause discomfort, pain, and difficulty swallowing, particularly in individuals with weakened immune systems or certain medical conditions. Treatment of oral thrush typically involves antifungal medications, oral hygiene measures, and management of underlying conditions to alleviate symptoms and prevent recurrence. If you suspect you have oral thrush or experience persistent symptoms such as white patches in the mouth or throat, it's important to consult a healthcare professional for evaluation and appropriate treatment.