Central Park Periodontics
Contact
Hours
<ul id=”hours” style=”transition: height .3s ease;”>
<li>Monday: 9:00am – 9:00pm</li>
<li>Tuesday: 9:00am – 6:00pm</li>
<li>Wednesday: 9:00am – 9:00pm</li>
<li>Thursday: 9:00am – 9:00pm</li>
<li>Friday: 9:00am – 5:00pm</li>
</ul>
Central Park Periodontics, located in the vibrant city of New York, NY, is a premier periodontal practice dedicated to providing exceptional care for patients seeking periodontal treatment and dental implant therapy. Led by a team of skilled periodontists and oral surgeons, Central Park Periodontics offers state-of-the-art treatments in a warm and welcoming environment, ensuring optimal oral health and beautiful smiles for every patient.
Periodontal Services
Gum Disease Treatment
- Comprehensive Evaluation: Thorough examination and diagnosis of gum disease to determine the most effective treatment approach.
- Scaling and Root Planing: Non-surgical deep cleaning to remove plaque and tartar from below the gumline and smooth the tooth roots.
- Periodontal Surgery: Surgical interventions such as flap surgery and bone grafting to treat advanced gum disease and restore periodontal health.
Dental Implant Therapy
- Implant Placement: Expert placement of dental implants to replace missing teeth and provide a stable foundation for crowns, bridges, or dentures.
- Bone Grafting: Bone augmentation procedures to rebuild bone structure and enhance the success of dental implant placement.
- Implant Restoration: Customized restoration of dental implants with lifelike crowns or prosthetic teeth for a natural-looking smile.
Advanced Procedures
Soft Tissue Grafting
- Gum Grafts: Surgical procedures to augment thin or receding gum tissue and improve gum aesthetics and function.
- Connective Tissue Grafts: Techniques to restore gum tissue lost due to periodontal disease or trauma, enhancing smile aesthetics and gum health.
Cosmetic Periodontics
- Gum Contouring: Reshaping of the gumline to create a more symmetrical and aesthetically pleasing smile.
- Crown Lengthening: Surgical procedure to expose more of the tooth’s surface, enhancing the appearance of short or gummy smiles.
Patient Care
Personalized Treatment Plans
- Customized Consultations: In-depth discussions and treatment planning sessions to address each patient’s unique oral health needs and goals.
- Collaborative Approach: Working closely with patients and their referring dentists to ensure coordinated and comprehensive care.
Comfort and Convenience
- Relaxing Environment: A welcoming atmosphere designed to help patients feel at ease during their visits.
- Sedation Options: Providing sedation dentistry options to help anxious patients relax and feel comfortable during treatment.
Mini Dental Implants
Mini dental implants (MDIs) are smaller diameter implants used to support dental restorations, such as crowns, bridges, or dentures. They are similar in function to traditional dental implants but have a smaller diameter, typically ranging from 1.8mm to 3.0mm, compared to standard implants which are typically 3.5mm or larger in diameter. Here's an overview of mini dental implants:
- Indications:
- Mini dental implants are commonly used to stabilize and support removable dental prostheses, such as dentures or overdentures, especially in cases where traditional implants are not feasible due to insufficient bone volume or other anatomical limitations.
- They may also be used to replace single missing teeth in areas with limited space or to support small fixed dental prostheses, such as single-tooth crowns or short-span bridges.
- Placement:
- The placement procedure for mini dental implants is similar to that of traditional implants, involving a surgical procedure to insert the implants into the jawbone.
- Mini implants require less invasive surgery compared to standard implants, as they require smaller incisions and typically involve less bone preparation.
- In some cases, mini implants can be placed using a flapless technique, which further reduces surgical trauma and recovery time.
- Osseointegration:
- After placement, mini dental implants undergo a process called osseointegration, during which they fuse with the surrounding bone tissue to provide stability and support.
- Osseointegration typically takes several months to complete, during which time the implants become firmly anchored in the jawbone.
- Restoration:
- Once osseointegration is complete, mini dental implants can be restored with dental prostheses, such as crowns, bridges, or dentures.
- Specialized attachments or abutments are used to secure the prostheses to the implants, providing stability and retention.
- Advantages:
- Mini dental implants offer several advantages over traditional implants, including:
- Less invasive surgery: Mini implants require smaller incisions and less bone preparation, resulting in reduced surgical trauma and faster recovery.
- Reduced cost: Mini implants are generally more cost-effective than traditional implants, making them a more affordable option for some patients.
- Versatility: Mini implants can be used in a variety of clinical situations, including cases where traditional implants are not feasible due to anatomical limitations or financial constraints.
- Considerations:
- While mini dental implants offer many benefits, they may not be suitable for all patients or clinical situations.
- The smaller diameter of mini implants may result in reduced stability and load-bearing capacity compared to traditional implants, particularly in cases of high bite forces or heavy chewing habits.
- Patient selection and case planning are crucial to the success of mini dental implant treatment, and careful consideration should be given to factors such as bone quality, occlusal forces, and esthetic requirements.
In summary, mini dental implants are smaller diameter implants used to support dental restorations, such as crowns, bridges, or dentures. They offer several advantages over traditional implants, including less invasive surgery, reduced cost, and versatility. However, careful patient selection and case planning are essential to ensure the success of mini dental implant treatment. If you are considering mini dental implants, it's important to consult with a qualified dental professional to determine the best treatment plan for your individual needs.
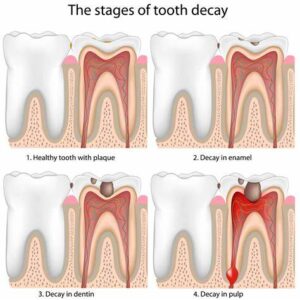
Tooth Decay
Tooth decay, also known as dental caries or cavities, is a common dental problem characterized by the breakdown of tooth structure due to the demineralization of enamel and dentin by acids produced by bacteria in the mouth. It is one of the most prevalent chronic diseases worldwide and can lead to pain, infection, and tooth loss if left untreated. Tooth decay occurs when the natural balance of bacteria in the mouth is disrupted, leading to the formation of plaque, a sticky film of bacteria and food particles that adheres to the teeth. The bacteria in plaque metabolize sugars and carbohydrates from food, producing acids that attack the tooth enamel and eventually lead to the formation of cavities.
Here are some key points about tooth decay:
- Causes:
- Bacteria: Oral bacteria, particularly Streptococcus mutans and Lactobacillus species, play a crucial role in the development of tooth decay by metabolizing sugars and carbohydrates from food and producing acids that demineralize tooth enamel.
- Diet: Consumption of sugary or carbohydrate-rich foods and beverages, such as candy, soda, fruit juice, and refined carbohydrates, provides fuel for bacteria in the mouth and contributes to the formation of plaque and tooth decay.
- Poor oral hygiene: Inadequate brushing, flossing, and tongue cleaning allow plaque to accumulate on the teeth, increasing the risk of tooth decay.
- Dry mouth: Reduced saliva flow, often caused by medications, medical conditions, or mouth breathing, can impair the natural cleansing and remineralization of teeth, increasing susceptibility to tooth decay.
- Genetics: Genetic factors may influence an individual's susceptibility to tooth decay, including the composition of saliva, tooth enamel structure, and immune response to bacteria.
- Stages:
- Initial demineralization: In the early stages of tooth decay, acids produced by bacteria in plaque attack the tooth enamel, causing demineralization and weakening of the enamel surface.
- Formation of cavities: As the enamel continues to demineralize, it may eventually break down, leading to the formation of small holes or cavities in the tooth surface.
- Progression of decay: If left untreated, tooth decay can progress deeper into the tooth, reaching the dentin layer and eventually the dental pulp, leading to pain, infection, and possible tooth loss.
- Symptoms:
- Tooth sensitivity: Sensitivity to hot, cold, sweet, or acidic foods and beverages is often an early sign of tooth decay.
- Toothache: Persistent or intermittent tooth pain, particularly when chewing or biting down, may indicate advanced tooth decay or infection.
- Visible holes or pits in the teeth: Cavities may be visible as dark spots, holes, or pits on the surface of the teeth.
- Discoloration: Discoloration or darkening of the teeth may occur as decay progresses and the enamel becomes thinner.
- Diagnosis:
- Diagnosis of tooth decay is typically based on a dental examination, evaluation of symptoms, and diagnostic tests such as dental X-rays or visual inspection with dental instruments.
- Your dentist will examine the teeth for signs of decay, including visible cavities, discoloration, or softening of the enamel.
- Dental X-rays may be taken to assess the extent of decay and detect cavities between the teeth or beneath the enamel surface.
- Treatment:
- Treatment of tooth decay aims to remove the decayed tissue, restore the tooth structure, and prevent further damage. Treatment options may include:
- Dental fillings: In cases of mild to moderate decay, your dentist may remove the decayed tissue and fill the cavity with a dental filling material such as composite resin, amalgam, or glass ionomer cement.
- Dental crowns: For more extensive decay or weakened teeth, your dentist may recommend placing a dental crown to restore the strength, function, and appearance of the tooth.
- Root canal therapy: If decay reaches the dental pulp and causes infection or inflammation, root canal therapy may be necessary to remove the infected tissue, clean and disinfect the root canal space, and seal it to prevent further infection.
- Tooth extraction: In cases of severe decay or irreparable damage, tooth extraction may be necessary to remove the affected tooth and prevent spread of infection to surrounding tissues.
- Prevention:
- To prevent tooth decay, it's important to:
- Practice good oral hygiene habits, including regular brushing with fluoride toothpaste, flossing, and tongue cleaning.
- Limit consumption of sugary or carbohydrate-rich foods and beverages that contribute to plaque formation and tooth decay.
- Drink water or chew sugar-free gum after meals to help rinse away food particles and neutralize acids in the mouth.
- Visit your dentist regularly for professional cleanings and check-ups to detect and treat tooth decay early.
In summary, tooth decay is a common dental problem characterized by the breakdown of tooth structure due to acid erosion by bacteria