Murray Hill Orthodontics
Contact
Hours
<ul id=”hours” style=”transition: height .3s ease;”>
<li>Monday: 9:00am – 9:00pm</li>
<li>Tuesday: 9:00am – 6:00pm</li>
<li>Wednesday: 9:00am – 9:00pm</li>
<li>Thursday: 9:00am – 9:00pm</li>
<li>Friday: 9:00am – 5:00pm</li>
</ul>
Murray Hill Orthodontics, located in the heart of New York, New York, is dedicated to providing exceptional orthodontic care in a warm and welcoming environment. Led by a team of experienced orthodontists, our practice combines personalized treatment plans with state-of-the-art technology to help patients achieve beautiful, healthy smiles. Whether you’re interested in traditional braces or clear aligners, Murray Hill Orthodontics offers a comprehensive range of orthodontic services to suit your needs.
Orthodontic Services
Traditional Braces
- Metal Braces: Time-tested orthodontic solution for correcting misaligned teeth and bite issues.
- Ceramic Braces: Clear or tooth-colored brackets for a more discreet orthodontic treatment option.
Clear Aligner Therapy
- Invisalign: Removable clear aligners for a virtually invisible way to straighten teeth without traditional braces.
- ClearCorrect: Transparent aligners that gradually shift teeth into alignment for a more aesthetically pleasing smile.
Comprehensive Orthodontic Care
Initial Consultation
- Orthodontic Evaluation: Thorough assessment to determine the most suitable treatment plan for your individual needs and goals.
- Customized Treatment Plan: Tailored orthodontic approach designed to achieve optimal results while considering your lifestyle and preferences.
Orthodontic Treatment
- Braces Adjustment: Regular visits to ensure braces or aligners are properly adjusted for consistent progress and comfort.
- Interceptive Orthodontics: Early intervention to address orthodontic issues in children and prevent more serious problems from developing.
Patient Experience
Comfortable Environment
- Modern Facility: State-of-the-art office equipped with advanced orthodontic technology for efficient and effective treatment.
- Relaxing Atmosphere: Comfortable and inviting environment to help patients feel at ease during their orthodontic appointments.
Personalized Care
- Individualized Attention: Dedicated orthodontic team committed to providing personalized care and addressing your specific concerns throughout your treatment journey.
- Open Communication: Transparent communication about your treatment plan, progress, and any adjustments needed to ensure the best possible outcome.
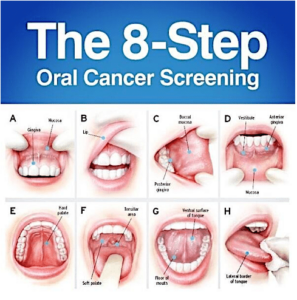
Oral Cancer Screening
Oral cancer screening is a preventive healthcare measure aimed at detecting signs and symptoms of oral cancer or precancerous lesions in the mouth, lips, tongue, gums, throat, or adjacent tissues at an early stage when treatment is most effective. Here's an overview of oral cancer screening and its key aspects:
- Importance of Oral Cancer Screening:
- Oral cancer is a serious and potentially life-threatening condition that can affect anyone, regardless of age, gender, or lifestyle factors. Early detection of oral cancer greatly improves the chances of successful treatment and survival.
- Oral cancer screening allows dentists and healthcare providers to identify suspicious lesions or abnormalities in the oral cavity that may indicate the presence of oral cancer or precancerous changes.
- Regular oral cancer screening is particularly important for individuals at higher risk, including tobacco users (smokers and smokeless tobacco users), heavy alcohol consumers, individuals with a family history of oral cancer, and those with human papillomavirus (HPV) infection.
- Screening Methods and Techniques:
- Oral cancer screening may be performed as part of a routine dental examination or as a standalone procedure during a visit to the dentist or healthcare provider.
- The screening process typically involves a visual examination of the oral cavity, lips, tongue, gums, throat, and adjacent tissues to look for any abnormalities, such as lumps, bumps, ulcers, red or white patches, or other suspicious lesions.
- In some cases, additional diagnostic tests or imaging studies, such as toluidine blue staining, brush biopsy, tissue biopsy, or imaging modalities like X-rays, CT scans, or MRI scans, may be recommended to further evaluate suspicious lesions and confirm or rule out the presence of cancer.
- Clinical Signs and Symptoms of Oral Cancer:
- During the oral cancer screening, the dentist or healthcare provider will look for the following signs and symptoms that may raise suspicion of oral cancer:
- Persistent mouth ulcers or sores that do not heal within two weeks.
- Red or white patches (leukoplakia or erythroplakia) on the oral mucosa.
- Unexplained swelling, lumps, or thickening of tissues in the mouth or neck.
- Pain, numbness, or difficulty swallowing (dysphagia).
- Chronic hoarseness or changes in voice quality.
- Persistent sore throat, ear pain, or jaw stiffness.
- Unexplained bleeding or numbness in the mouth.
- Risk Factors for Oral Cancer:
- Several factors increase the risk of developing oral cancer, including:
- Tobacco Use: Smoking cigarettes, cigars, pipes, or using smokeless tobacco products (chewing tobacco, snuff) greatly increases the risk of oral cancer.
- Heavy Alcohol Consumption: Excessive alcohol consumption, especially when combined with tobacco use, significantly raises the risk of oral cancer.
- HPV Infection: Certain strains of human papillomavirus (HPV), particularly HPV-16 and HPV-18, have been linked to an increased risk of oral and oropharyngeal cancers.
- Sun Exposure: Prolonged exposure to ultraviolet (UV) radiation from the sun or tanning beds increases the risk of lip cancer.
- Age and Gender: Oral cancer tends to occur more frequently in older adults over the age of 50 and is more common in men than women.
- Preventive Measures and Follow-up:
- While oral cancer screening can help detect early signs of oral cancer, prevention is key to reducing the risk of developing the disease.
- Individuals can reduce their risk of oral cancer by avoiding tobacco use, moderating alcohol consumption, practicing good oral hygiene, eating a healthy diet rich in fruits and vegetables, and minimizing exposure to known risk factors.
- Regular dental check-ups and oral cancer screenings are essential for early detection and prompt treatment of oral cancer. Patients should follow up with their dentist or healthcare provider if they notice any changes or abnormalities in their oral health between screenings.
In summary, oral cancer screening is a vital component of preventive healthcare aimed at detecting oral cancer and precancerous lesions at an early stage when treatment is most effective. By undergoing regular screenings, individuals can reduce their risk of developing oral cancer and improve their chances of successful treatment and recovery.
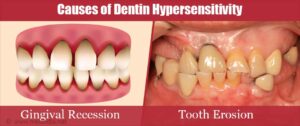
Dentin Hypersensitivity
Dentin hypersensitivity, also known as tooth sensitivity, is a common dental condition characterized by sharp, sudden pain or discomfort in response to certain stimuli, such as hot, cold, sweet, or acidic foods and beverages, as well as touch or pressure. It occurs when the dentin, the layer of tissue underlying the enamel and cementum, becomes exposed or irritated, leading to increased sensitivity of the teeth.
Here are some key points about dentin hypersensitivity:
- Anatomy of Dentin: Dentin is a hard tissue that makes up the bulk of the tooth structure beneath the enamel and cementum. It contains microscopic tubules that extend from the outer surface of the tooth to the pulp (nerve) chamber. When dentin becomes exposed due to enamel wear, gum recession, or loss of cementum, these tubules can transmit external stimuli to the nerves in the pulp, resulting in pain or discomfort.
- Causes of Dentin Hypersensitivity: Dentin hypersensitivity can be caused by various factors that lead to exposure or irritation of the dentin. Common causes include:
- Gum recession: Receding gums can expose the sensitive root surfaces of the teeth, making them more susceptible to external stimuli.
- Enamel erosion: Acidic foods and beverages, frequent consumption of acidic drinks, or gastroesophageal reflux disease (GERD) can lead to erosion of the enamel, exposing the underlying dentin.
- Tooth wear: Abrasive toothbrushing, tooth grinding (bruxism), or abrasive toothpaste can wear down the enamel and expose the dentin.
- Dental procedures: Certain dental treatments such as tooth whitening, tooth restoration, or periodontal procedures may temporarily increase tooth sensitivity.
- Clinical Presentation: Dentin hypersensitivity typically presents with the following signs and symptoms:
- Sharp, sudden pain or discomfort in response to hot, cold, sweet, or acidic foods and beverages.
- Sensitivity to touch or pressure, particularly when brushing or flossing the teeth.
- Discomfort or pain that subsides quickly once the stimulus is removed.
- Preference for avoiding certain foods or drinks that trigger sensitivity.
- Increased sensitivity during cold weather or exposure to cold air.
- Diagnosis: Diagnosis of dentin hypersensitivity involves a thorough clinical examination, assessment of dental history, and identification of potential causative factors. Dental X-rays or other diagnostic tests may be performed to evaluate the extent of tooth wear, gum recession, or other structural changes contributing to sensitivity.
- Treatment: Treatment of dentin hypersensitivity aims to alleviate symptoms, reduce tooth sensitivity, and prevent further enamel loss or dentin exposure. Management options may include:
- Desensitizing toothpaste: Use of specially formulated toothpaste containing desensitizing agents such as potassium nitrate, fluoride, or calcium phosphate to block the transmission of nerve impulses and reduce tooth sensitivity.
- Fluoride therapy: Application of fluoride varnishes, gels, or rinses to strengthen the enamel, remineralize the tooth surface, and reduce sensitivity.
- Dental sealants: Application of dental sealants or bonding materials to cover exposed root surfaces and protect against external stimuli.
- Gum grafting: Surgical procedure to repair gum recession and cover exposed root surfaces, particularly in cases of severe gum recession.
- Avoidance of triggering factors: Counseling on dietary modifications, oral hygiene practices, and lifestyle changes to minimize exposure to acidic or abrasive substances and reduce the risk of tooth sensitivity.
In summary, dentin hypersensitivity is a common dental condition characterized by sharp, sudden pain or discomfort in response to certain stimuli. It can result from various factors that lead to exposure or irritation of the dentin, such as gum recession, enamel erosion, tooth wear, or dental procedures. Diagnosis and treatment of dentin hypersensitivity require a comprehensive approach to identify underlying causes and implement appropriate management strategies to alleviate symptoms and improve oral comfort.