What is it?
Root resorption is a pathological process characterized by the breakdown or loss of dentin, cementum, and/or bone in the root of a tooth. It can occur as a result of various factors and may involve either external resorption, which affects the outer surface of the root, or internal resorption, which affects the pulp chamber and root canal system within the tooth.
Here are some key points about root resorption:
- Types of Root Resorption:
- External Resorption: External resorption, also known as external inflammatory resorption, typically occurs in response to trauma, orthodontic treatment, periodontal disease, or excessive mechanical forces. It involves the breakdown of cementum and dentin on the outer surface of the root and may progress slowly over time if left untreated.
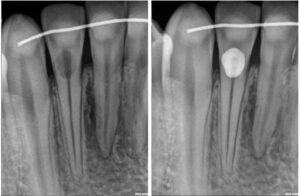
- Internal Resorption: Internal resorption, also known as internal inflammatory resorption, occurs within the pulp chamber and root canal system of the tooth. It can be caused by trauma, chronic pulp inflammation, pulpal necrosis, or excessive orthodontic forces. Internal resorption is often asymptomatic and may be detected incidentally on dental radiographs.
- Causes of Root Resorption:
- Trauma: Dental trauma, such as falls, sports injuries, or accidents, can lead to root resorption, particularly if the tooth sustains a significant impact or fracture.
- Orthodontic Treatment: Orthodontic forces applied during tooth movement can sometimes lead to localized areas of root resorption, particularly in cases of prolonged or excessive force application.
- Periodontal Disease: Advanced periodontal disease or inflammation can cause destruction of the supporting structures of the tooth, leading to root resorption.
- Pulpal Pathology: Chronic pulp inflammation, pulp necrosis, or periapical infection can initiate internal resorption within the pulp chamber and root canal system.
- Clinical Presentation:
- External resorption may present with symptoms such as tooth mobility, sensitivity to percussion or palpation, localized swelling, or changes in tooth position.
- Internal resorption is often asymptomatic and may be detected incidentally on dental radiographs during routine dental examinations.
- Severe or advanced cases of root resorption may lead to tooth fracture, pulp exposure, or loss of tooth vitality.
- Diagnosis:
- Diagnosis of root resorption involves a comprehensive clinical examination, assessment of dental history, and evaluation of dental radiographs or imaging studies.
- Dental radiographs, including periapical radiographs or cone-beam computed tomography (CBCT), are essential for visualizing the extent and location of root resorption and determining appropriate treatment options.
- Treatment:
- The treatment approach for root resorption depends on the cause, extent, and severity of the resorption.
- In cases of external resorption, treatment may involve stabilization of the tooth, elimination of causative factors (e.g., orthodontic forces), and surgical intervention to remove affected tissue and restore the root structure.
- Internal resorption may require endodontic treatment (root canal therapy) to remove necrotic tissue, disinfect the root canal system, and seal the resorptive defect with biocompatible materials.
- Severe or advanced cases of root resorption may necessitate tooth extraction followed by replacement with a dental implant, bridge, or removable prosthesis.
In summary, root resorption is a pathological process characterized by the breakdown or loss of dentin, cementum, and/or bone in the root of a tooth. It can occur due to various factors such as trauma, orthodontic treatment, periodontal disease, or pulpal pathology. Diagnosis and treatment of root resorption require a thorough evaluation and may involve stabilization of the tooth, removal of causative factors, endodontic treatment, or tooth extraction followed by replacement with a dental prosthesis. Early detection and intervention are essential for preserving tooth structure and function and preventing complications associated with root resorption.